Peptic ulcer
| Peptic ulcer | |
|---|---|
| Classification and external resources | |
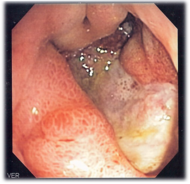 Deep gastric ulcer |
|
| ICD-10 | K25.-K27. |
| ICD-9 | 531-534 |
| DiseasesDB | 9819 |
| eMedicine | med/1776 ped/2341 |
| MeSH | D010437 |
A peptic ulcer, also known as ulcus pepticum, PUD or peptic ulcer disease,[1] is an ulcer (defined as mucosal erosions equal to or greater than 0.5 cm) of an area of the gastrointestinal tract that is usually acidic and thus extremely painful. As many as 70-90% of ulcers are associated with Helicobacter pylori, a spiral-shaped bacterium that lives in the acidic environment of the stomach, however only 40% of those cases go to a doctor. Ulcers can also be caused or worsened by drugs such as aspirin and other NSAIDs.
Contrary to general belief, more peptic ulcers arise in the duodenum (first part of the small intestine, just after the stomach) rather than in the stomach. About 4% of stomach ulcers are caused by a malignant tumor, so multiple biopsies are needed to exclude cancer. Duodenal ulcers are generally benign.
Contents |
Classification
- Stomach (called gastric ulcer)
- Duodenum (called duodenal ulcer)
- Oesophagus (called Oesophageal ulcer)
- Meckel's Diverticulum (called Meckel's Diverticulum ulcer)
Types of peptic ulcers:
- Type I: Ulcer along the lesser curve of stomach
- Type II: Two ulcers present - one gastric, one duodenal
- Type III: Prepyloric ulcer
- Type IV: Proximal gastroesophageal ulcer
- Type V: Anywhere
Signs and symptoms
Symptoms of a peptic ulcer can be
- abdominal pain, classically epigastric with severity relating to mealtimes, after around 3 hours of taking a meal (duodenal ulcers are classically relieved by food, while gastric ulcers are exacerbated by it);
- bloating and abdominal fullness;
- waterbrash (rush of saliva after an episode of regurgitation to dilute the acid in esophagus);
- nausea, and copious vomiting;
- loss of appetite and weight loss;
- hematemesis (vomiting of blood); this can occur due to bleeding directly from a gastric ulcer, or from damage to the esophagus from severe/continuing vomiting.
- melena (tarry, foul-smelling feces due to oxidized iron from hemoglobin);
- rarely, an ulcer can lead to a gastric or duodenal perforation, which leads to acute peritonitis. This is extremely painful and requires immediate surgery.
A history of heartburn, gastroesophageal reflux disease (GERD) and use of certain forms of medication can raise the suspicion for peptic ulcer. Medicines associated with peptic ulcer include NSAID (non-steroid anti-inflammatory drugs) that inhibit cyclooxygenase, and most glucocorticoids (e.g. dexamethasone and prednisolone).
In patients over 45 with more than two weeks of the above symptoms, the odds for peptic ulceration are high enough to warrant rapid investigation by EGD (see below).
The timing of the symptoms in relation to the meal may differentiate between gastric and duodenal ulcers: A gastric ulcer would give epigastric pain during the meal, as gastric acid is secreted, or after the meal, as the alkaline duodenal contents reflux into the stomach. Symptoms of duodenal ulcers would manifest mostly before the meal—when acid (production stimulated by hunger) is passed into the duodenum. However, this is not a reliable sign in clinical practice.
Also, the symptoms of peptic ulcers may vary with the location of the ulcer and the patient's age. Furthermore, typical ulcers tend to heal and recur and as a result the pain may occur for few days and weeks and then wane or disappear.[2] Usually, children and the elderly do not develop any symptoms unless complications have arisen.
Burning or gnawing feeling in the stomach area lasting between 30 minutes and 3 hours commonly accompanies ulcers. This pain can be misinterpreted as hunger, indigestion or heartburn. Pain is usually caused by the ulcer but it may be aggravated by the stomach acid when it comes into contact with the ulcerated area. The pain caused by peptic ulcers can be felt anywhere from the navel up to the breastbone, it may last from few minutes to several hours and it may be worse when the stomach is empty. Also, sometimes the pain may flare at night and it can commonly be temporarily relived by eating foods that buffer stomach acid or by taking anti-acid medication.[3] However, peptic ulcer disease symptoms may be different for every sufferer.[4]
Complications
- Gastrointestinal bleeding is the most common complication. Sudden large bleeding can be life-threatening.[5] It occurs when the ulcer erodes one of the blood vessels.
- Perforation (a hole in the wall) often leads to catastrophic consequences. Erosion of the gastro-intestinal wall by the ulcer leads to spillage of stomach or intestinal content into the abdominal cavity. Perforation at the anterior surface of the stomach leads to acute peritonitis, initially chemical and later bacterial peritonitis. The first sign is often sudden intense abdominal pain. Posterior wall perforation leads to pancreatitis; pain in this situation often radiates to the back.
- Penetration is when the ulcer continues into adjacent organs such as the liver and pancreas.[6]
- Scarring and swelling due to ulcers causes narrowing in the duodenum and gastric outlet obstruction. Patient often presents with severe vomiting.
- Cancer is included in the differential diagnosis (elucidated by biopsy), Helicobacter pylori as the etiological factor making it 3 to 6 times more likely to develop stomach cancer from the ulcer.[7]
Cause
A major causative factor (60% of gastric and up to 90% of duodenal ulcers) is chronic inflammation due to Helicobacter pylori that colonizes the antral mucosa. The immune system is unable to clear the infection, despite the appearance of antibodies. Thus, the bacterium can cause a chronic active gastritis (type B gastritis), resulting in a defect in the regulation of gastrin production by that part of the stomach, and gastrin secretion can either be decreased (most cases) resulting in hypo- or achlorhydria or increased. Gastrin stimulates the production of gastric acid by parietal cells and, in H. pylori colonization responses that increase gastrin, the increase in acid can contribute to the erosion of the mucosa and therefore ulcer formation.
Another major cause is the use of NSAIDs (see above). The gastric mucosa protects itself from gastric acid with a layer of mucus, the secretion of which is stimulated by certain prostaglandins. NSAIDs block the function of cyclooxygenase 1 (cox-1), which is essential for the production of these prostaglandins. COX-2 selective anti-inflammatories (such as celecoxib or the since withdrawn rofecoxib) preferentially inhibit cox-2, which is less essential in the gastric mucosa, and roughly halve the risk of NSAID-related gastric ulceration. As the prevalence of H. pylori-caused ulceration declines in the Western world due to increased medical treatment, a greater proportion of ulcers will be due to increasing NSAID use among individuals with pain syndromes as well as the growth of aging populations that develop arthritis.
The incidence of duodenal ulcers has dropped significantly during the last 30 years, while the incidence of gastric ulcers has shown a small increase, mainly caused by the widespread use of NSAIDs. The drop in incidence is considered to be a cohort-phenomenon independent of the progress in treatment of the disease. The cohort-phenomenon is probably explained by improved standards of living which has lowered the incidence of H. pylori infections.[8]
Although some studies have found correlations between smoking and ulcer formation [9], others have been more specific in exploring the risks involved and have found that smoking by itself may not be much of a risk factor unless associated with H. pylori infection [10][11][12] [nb 1]. Some suggested risk factors such as diet, spice, consumption and blood type, were hypothesized as ulcerogens (helping cause ulcers) until late in the 20th century, but have been shown to be of relatively minor importance in the development of peptic ulcers.[13]. Similarly, while studies have found that alcohol consumption increases risk when associated with H. pylori infection, it does not seem to independently increase risk, and even when coupled with H. pylori infection, the increase is modest in comparison to the primary risk factor [10][14][nb 2].
Gastrinomas (Zollinger Ellison syndrome), rare gastrin-secreting tumors, also cause multiple and difficult to heal ulcers.
Stress
Researchers also continue to look at stress as a possible cause, or at least complication, in the development of ulcers. There is debate as to whether psychological stress can influence the development of peptic ulcers. Burns and head trauma, however, can lead to physiologic stress ulcers, which are reported in many patients who are on mechanical ventilation.
An expert panel convened by the Academy of Behavioral Medicine Research concluded that ulcers are not purely an infectious disease and that psychological factors do play a significant role.[1] Researchers are examining how stress might promote H. pylori infection. For example, Helicobacter pylori thrives in an acidic environment, and stress has been demonstrated to cause the production of excess stomach acid. This was supported by a study on mice showing that both long-term water-immersion-restraint stress and H. pylori infection were independently associated with the development of peptic ulcers.[15]
A study of peptic ulcer patients in a Thai hospital showed that chronic stress was strongly associated with an increased risk of peptic ulcer, and a combination of chronic stress and irregular mealtimes was a significant risk factor.[16]
Diagnosis

The diagnosis is mainly established based on the characteristic symptoms. The stomach pain is usually the first to signal a peptic ulcer. In some cases, doctors may treat ulcers without diagnosing them with specific tests and observe if the symptoms resolve, meaning their primary diagnosis was accurate.
Confirming the diagnosis is made with the help of tests such as endoscopies or barium contrast x-rays. The tests are typically ordered if the symptoms do not resolve after a few weeks of treatment, or when they first appear in a person who is over age 45 or who has other symptoms such as weight loss, because stomach cancer can cause similar symptoms. Also, when severe ulcers resist treatment, particularly if a person has several ulcers or the ulcers are in unusual places, a doctor may suspect an underlying condition that causes the stomach to overproduce acid.[2]
An esophagogastroduodenoscopy (EGD), a form of endoscopy, also known as a gastroscopy, is carried out on patients in whom a peptic ulcer is suspected. By direct visual identification, the location and severity of an ulcer can be described. Moreover, if no ulcer is present, EGD can often provide an alternative diagnosis.
One of the reasons why blood tests are not reliable on establishing an accurate peptic ulcer diagnosis on their own is their inability to differentiate between past exposure to the bacteria and current infection. Additionally, a false-negative is possible with a blood test if the patient has recently been taking certain drugs, such as antibiotics or proton pump inhibitors.[17]
The diagnosis of Helicobacter pylori can be made by:
- Urea breath test (noninvasive and does not require EGD);
- Direct culture from an EGD biopsy specimen; this is difficult to do, and can be expensive. Most labs are not set up to perform H. pylori cultures;
- Direct detection of urease activity in a biopsy specimen by rapid urease test;
- Measurement of antibody levels in blood (does not require EGD). It is still somewhat controversial whether a positive antibody without EGD is enough to warrant eradication therapy;
- Stool antigen test;
- Histological examination and staining of an EGD biopsy.
The breath test uses radioactive carbon atom to detect H. pylori.[18] To perform this exam the patient will be asked to drink a tasteless liquid which contains the carbon as part of the substance that the bacteria breaks down. After an hour, the patient will be asked to blow into a bag that is sealed. If the patient is infected with H. pylori, the breath sample will contain carbon dioxide. This test provides the advantage of being able to monitor the response to treatment used to kill the bacteria.
The possibility of other causes of ulcers, notably malignancy (gastric cancer) needs to be kept in mind. This is especially true in ulcers of the greater (large) curvature of the stomach; most are also a consequence of chronic H. pylori infection.
If a peptic ulcer perforates, air will leak from the inside of the gastrointestinal tract (which always contains some air) to the peritoneal cavity (which normally never contains air). This leads to "free gas" within the peritoneal cavity. If the patient stands erect, as when having a chest X-ray, the gas will float to a position underneath the diaphragm. Therefore, gas in the peritoneal cavity, shown on an erect chest X-ray or supine lateral abdominal X-ray, is an omen of perforated peptic ulcer disease.
Macroscopic appearance

Gastric ulcers are most often localized on the lesser curvature of the stomach. The ulcer is a round to oval parietal defect ("hole"), 2 to 4 cm diameter, with a smooth base and perpendicular borders. These borders are not elevated or irregular in the acute form of peptic ulcer, regular but with elevated borders and inflammatory surrounding in the chronic form. In the ulcerative form of gastric cancer the borders are irregular. Surrounding mucosa may present radial folds, as a consequence of the parietal scarring.
Microscopic appearance
A gastric peptic ulcer is a mucosal defect which penetrates the muscularis mucosae and muscularis propria, produced by acid-pepsin aggression. Ulcer margins are perpendicular and present chronic gastritis. During the active phase, the base of the ulcer shows 4 zones: inflammatory exudate, fibrinoid necrosis, granulation tissue and fibrous tissue. The fibrous base of the ulcer may contain vessels with thickened wall or with thrombosis.[19]
Differential diagnosis of epigastric pain
- Peptic ulcer
- Gastritis
- Stomach cancer
- Gastroesophageal reflux disease
- Pancreatitis
- Hepatic congestion
- Cholecystitis
- Biliary colic
- Inferior myocardial infarction
- Referred pain (pleurisy, pericarditis)
- Superior mesenteric artery syndrome
Treatment
Younger patients with ulcer-like symptoms are often treated with antacids or H2 antagonists before EGD is undertaken. Bismuth compounds may actually reduce or even clear organisms, though the warning labels of some bismuth subsalicylate products indicate that the product should not be used by someone with an ulcer.
Patients who are taking nonsteroidal anti-inflammatories (NSAIDs) may also be prescribed a prostaglandin analogue (Misoprostol) in order to help prevent peptic ulcers, which may be a side-effect of the NSAIDs.
When H. pylori infection is present, the most effective treatments are combinations of 2 antibiotics (e.g. Clarithromycin, Amoxicillin, Tetracycline, Metronidazole) and 1 proton pump inhibitor (PPI), sometimes together with a bismuth compound. In complicated, treatment-resistant cases, 3 antibiotics (e.g. amoxicillin + clarithromycin + metronidazole) may be used together with a PPI and sometimes with bismuth compound. An effective first-line therapy for uncomplicated cases would be Amoxicillin + Metronidazole + Pantoprazole (a PPI). In the absence of H. pylori, long-term higher dose PPIs are often used.
Treatment of H. pylori usually leads to clearing of infection, relief of symptoms and eventual healing of ulcers. Recurrence of infection can occur and retreatment may be required, if necessary with other antibiotics. Since the widespread use of PPI's in the 1990s, surgical procedures (like "highly selective vagotomy") for uncomplicated peptic ulcers became obsolete.
Perforated peptic ulcer is a surgical emergency and requires surgical repair of the perforation. Most bleeding ulcers require endoscopy urgently to stop bleeding with cautery, injection, or clipping.
Epidemiology

The lifetime risk for developing a peptic ulcer is approximately 10%.[21]
In Western countries the prevalence of Helicobacter pylori infections roughly matches age (i.e., 20% at age 20, 30% at age 30, 80% at age 80 etc). Prevalence is higher in third world countries. Transmission is by food, contaminated groundwater, and through human saliva (such as from kissing or sharing food utensils.)
A minority of cases of Helicobacter infection will eventually lead to an ulcer and a larger proportion of people will get non-specific discomfort, abdominal pain or gastritis.
Peptic ulcer disease had a tremendous effect on morbidity and mortality until the last decades of the 20th century, when epidemiological trends started to point to an impressive fall in its incidence.[22] The reason why the rates of peptic ulcer disease decreased is thought to be the development of new effective medication and acid suppressants and the discovery of the cause of the condition, H. pylori.
In the United States about 4 million people have active peptic ulcers and about 350,000 new cases are diagnosed each year. Four times as many duodenal ulcers as gastric ulcers are diagnosed. Approximately 3,000 deaths per year in the United States are due to duodenal ulcer and 3,000 to gastric ulcer.[23]
History
John Lykoudis, a general practitioner in Greece, treated patients for peptic ulcer disease with antibiotics, beginning in 1958, long before it was commonly recognized that bacteria were a dominant cause for the disease.[24]
Helicobacter pylori was rediscovered in 1982 by two Australian scientists, Robin Warren and Barry J. Marshall as a causative factor for ulcers.[25] In their original paper, Warren and Marshall contended that most stomach ulcers and gastritis were caused by colonization with this bacterium, not by stress or spicy food as had been assumed before.[26]
The H. pylori hypothesis was poorly received, so in an act of self-experimentation Marshall drank a Petri dish containing a culture of organisms extracted from a patient and soon developed gastritis. His symptoms disappeared after two weeks, but he took antibiotics to kill the remaining bacteria at the urging of his wife, since halitosis is one of the symptoms of infection.[27] This experiment was published in 1984 in the Australian Medical Journal and is among the most cited articles from the journal.
In 1997, the Centers for Disease Control and Prevention, with other government agencies, academic institutions, and industry, launched a national education campaign to inform health care providers and consumers about the link between H. pylori and ulcers. This campaign reinforced the news that ulcers are a curable infection, and that health can be greatly improved and money saved by disseminating information about H. pylori.[28]
In 2005, the Karolinska Institute in Stockholm awarded the Nobel Prize in Physiology or Medicine to Dr. Marshall and his long-time collaborator Dr. Warren "for their discovery of the bacterium Helicobacter pylori and its role in gastritis and peptic ulcer disease". Professor Marshall continues research related to H. pylori and runs a molecular biology lab at UWA in Perth, Western Australia.
It was a previously widely accepted misunderstanding that the use of chewing gum resulted in gastric ulcers. The medical profession believed that this was because the action of masticating on gum caused the over-stimulation of the production of hydrochloric acid in the stomach. The low (acidic) pH (pH 2), or hyperchlorhydria was then believed to cause erosion of the stomach lining in the absence of food, thus causing the development of the gastric ulcers.[29]
On the other hand, in the recent past, some believed that natural tree resin extract, mastic gum, actively eliminates the H. pylori bacteria.[30] However, multiple subsequent studies have found no effect of using mastic gum on reducing H. pylori levels.[31][32]
Notes
- ↑ Kurata 1997 explains that "Data in Fig. 8 indicate that 89% of all serious upper GI disease can be accounted for by NSAIDs and H. pylori, with cigarette smoking acting as a synergistic co-factor."(14)
- ↑ Sonnenberg in his study cautiously concludes that, among other potential factors that were found to correlate to ulcer healing, "moderate alcohol intake might [also] favor ulcer healing" (p. 1066)
References
- ↑ 1.0 1.1 "GI Consult: Perforated Peptic Ulcer". http://www.emedmag.com/html/pre/gic/consults/071503.asp. Retrieved 2007-08-26.
- ↑ 2.0 2.1 "Peptic Ulcer". http://www.merck.com/mmhe/sec09/ch121/ch121c.html. Retrieved 2010-06-18.
- ↑ "Peptic ulcer". http://www.mayoclinic.com/health/peptic-ulcer/ds00242/dsection=symptoms. Retrieved 2010-06-18.
- ↑ "Ulcer Disease Facts and Myths". http://www.ulcerdisease.net/. Retrieved 2010-06-18.
- ↑ Cullen DJ, Hawkey GM, Greenwood DC, et al. (1997). "Peptic ulcer bleeding in the elderly: relative roles of Helicobacter pylori and non-steroidal anti-inflammatory drugs". Gut 41 (4): 459–62. doi:10.1136/gut.41.4.459. PMID 9391242. PMC 1891536. http://gut.bmj.com/cgi/pmidlookup?view=long&pmid=9391242.
- ↑ "Peptic Ulcer: Peptic Disorders: Merck Manual Home Edition". http://www.merck.com/mmhe/sec09/ch121/ch121c.html. Retrieved 2007-10-10.
- ↑ http://www.merck.com/mmhe/sec09/ch121/ch121c.html
- ↑ Johannessen T. "Peptic ulcer disease". Pasienthandboka. http://www.pasienthandboka.no/default.asp?mode=document&parentid=2104&menuid=2105&documentid=26957.
- ↑ Kato, Ikuko; Abraham M. Y. Nomura, Grant N. Stemmermann and Po-Huang Chyou (1992). "A Prospective Study of Gastric and Duodenal Ulcer and Its Relation to Smoking, Alcohol, and Diet". American Journal of Epidemiology 135 (5): 521–530. PMID 1570818. http://aje.oxfordjournals.org/cgi/content/abstract/135/5/521. Retrieved 2010-03-18.
- ↑ 10.0 10.1 Salih, Barik; M Fatih Abasiyanik, Nizamettin Bayyurt, Ersan Sander (June 2007). "H pylori infection and other risk factors associated with peptic ulcers in Turkish patients: A retrospective study". World Journal of Gastroenterology 13 (23): 3245–3248. PMID 17589905.
- ↑ Martin, U.S.A.F.M.C. (Major), David F.; Captain Elizabeth Montgomery, U.S.A. M.C., Arthus S, Dobek, Ph.D., Geoffrey A, Patrissi, M.A., Colonel David A, Peura, U.S.A. M.C., F.A.C.G. (28 Jun 2008). "Campylobacter pylori, NSAIDS, and Smoking: Risk Factors for Peptic Ulcer Disease". American Journal of Gastroenterology 84 (10): 1268–1272. doi:10.1111/j.1572-0241.1989.tb06166.x. PMID 2801677. http://www3.interscience.wiley.com/journal/120151138/abstract?CRETRY=1&SRETRY=0. Retrieved 2010-03-18.
- ↑ Kurata Ph.D.,M.P.H., John H.; Nogawa, Aki N. M.S. (Jan 1997). "Meta-analysis of Risk Factors for Peptic Ulcer: Nonsteroidal Antiinflammatory Drugs, Helicobacter pylori, and Smoking". Journal of Clinical Gastroenterology 24 (1): 2–17. doi:10.1097/00004836-199701000-00002. PMID 9013343. http://journals.lww.com/jcge/Abstract/1997/01000/Meta_analysis_of_Risk_Factors_for_Peptic_Ulcer_.2.aspx. Retrieved 2010-03-18.
- ↑ For nearly 100 years, scientists and doctors thought that ulcers were caused by stress, spicy food, and alcohol. Treatment involved bed rest and a bland diet. Later, researchers added stomach acid to the list of causes and began treating ulcers with antacids. National Digestive Diseases Information Clearinghouse
- ↑ A, Sonnenberg; Müller-Lissner SA, Vogel E, Schmid P, Gonvers JJ, Peter P, Strohmeyer G, Blum AL (1981). "Predictors of duodenal ulcer healing and relapse.". Journal of Gastroenterology 81 (6): 1061–1067. PMID 7026344. http://www.gastrojournal.org/article/S0016-5085(81)70048-9/abstract. Retrieved 2010-03-18.
- ↑ Kim YH, Lee JH, Lee SS, et al. (2002). "Long-term stress and Helicobacter pylori infection independently induce gastric mucosal lesions in C57BL/6 mice". Scand. J. Gastroenterol. 37 (11): 1259–64. doi:10.1080/003655202761020515. PMID 12465722.
- ↑ Wachirawat W, Hanucharurnkul S, Suriyawongpaisal P, et al. (2003). "Stress, but not Helicobacter pylori, is associated with peptic ulcer disease in a Thai population". J Med Assoc Thai 86 (7): 672–85. PMID 12948263.
- ↑ "Peptic ulcer". http://www.mayoclinic.com/health/peptic-ulcer/DS00242/DSECTION=tests-and-diagnosis. Retrieved 2010-06-18.
- ↑ "Tests and diagnosis". http://www.mayoclinic.com/health/peptic-ulcer/DS00242/DSECTION=tests-and-diagnosis. Retrieved 2010-06-18.
- ↑ "ATLAS OF PATHOLOGY". http://www.pathologyatlas.ro/chronic-peptic-ulcer.php. Retrieved 2007-08-26.
- ↑ "WHO Disease and injury country estimates". World Health Organization. 2009. http://www.who.int/healthinfo/global_burden_disease/estimates_country/en/index.html. Retrieved Nov. 11, 2009.
- ↑ Snowden FM (October 2008). "Emerging and reemerging diseases: a historical perspective". Immunol. Rev. 225: 9–26. doi:10.1111/j.1600-065X.2008.00677.x. PMID 18837773.
- ↑ "Peptic ulcer disease". http://lib.bioinfo.pl/meid:32219. Retrieved 2010-06-18.
- ↑ "Epidemiology of peptic ulcer disease". http://www.ncbi.nlm.nih.gov/pubmed/6378441. Retrieved 2010-06-18.
- ↑ Marshall B.J., ed. (2002), "Helicobacter Pioneers: Firsthand accounts from the scientists who discovered helicobacters, 1892–1982", ISBN 0-86793-035-7. Basil Rigas, Efstathios D. Papavasassiliou. John Lykoudis. The general practitioner in Greece who in 1958 discovered the etiology of, and a treatment for, peptic ulcer disease.
- ↑ Marshall B.J. (1983). "Unidentified curved bacillus on gastric epithelium in active chronic gastritis". Lancet 1 (8336): 1273–5. PMID 6134060.
- ↑ Marshall B.J., Warren J.R. (1984). "Unidentified curved bacilli in the stomach patients with gastritis and peptic ulceration". Lancet 1 (8390): 1311–5. doi:10.1016/S0140-6736(84)91816-6. PMID 6145023.
- ↑ Van Der Weyden MB, Armstrong RM, Gregory AT (2005). "The 2005 Nobel Prize in physiology or medicine". Med. J. Aust. 183 (11–12): 612–4. PMID 16336147. http://www.mja.com.au/public/issues/183_11_051205/van11000_fm.html#0_i1091639.
- ↑ Ulcer, Diagnosis and Treatment - CDC Bacterial, Mycotic Diseases
- ↑ Medicine for Nurses (Toohey, 1974)
- ↑ Huwez FU, Thirlwell D, Cockayne A, Ala'Aldeen DA (December 1998). "Mastic gum kills Helicobacter pylori [Letter to the editor, not a peer-reviewed scientific article"]. N. Engl. J. Med. 339 (26): 1946. doi:10.1056/NEJM199812243392618. PMID 9874617. http://content.nejm.org/cgi/content/extract/339/26/1946. Retrieved 2008-09-06. See also their corrections in the next volume.
- ↑ Loughlin MF, Ala'Aldeen DA, Jenks PJ (February 2003). "Monotherapy with mastic does not eradicate Helicobacter pylori infection from mice". J. Antimicrob. Chemother. 51 (2): 367–71. doi:10.1093/jac/dkg057. PMID 12562704. http://jac.oxfordjournals.org/cgi/pmidlookup?view=long&pmid=12562704.
- ↑ Bebb JR, Bailey-Flitter N, Ala'Aldeen D, Atherton JC (September 2003). "Mastic gum has no effect on Helicobacter pylori load in vivo". J. Antimicrob. Chemother. 52 (3): 522–3. doi:10.1093/jac/dkg366. PMID 12888582. http://jac.oxfordjournals.org/cgi/pmidlookup?view=long&pmid=12888582.
External links
- Endoscopy Video of a deep gastric ulcer
- Gastric Ulcer Radiology and Endoscopy from MedPix
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||